Riverside Health is advancing lung cancer care across Eastern Virginia through the use of Single Anesthesia Bronchoscopy and Resection (SABR) — an innovative, coordinated approach that combines diagnosis and surgical treatment for lung cancer into a single procedure. Riverside’s expert thoracic and pulmonary teams have already successfully completed multiple SABR procedures at Riverside Regional Medical Center.

SABR brings together two key steps — bronchoscopy to help in marking the lung area and lung resection surgery—into one carefully planned operation under a single round of anesthesia. Traditionally performed days or weeks apart, combining these procedures enables Riverside to move swiftly from diagnosis to treatment without requiring the patient to undergo anesthesia twice or wait for separate appointments.
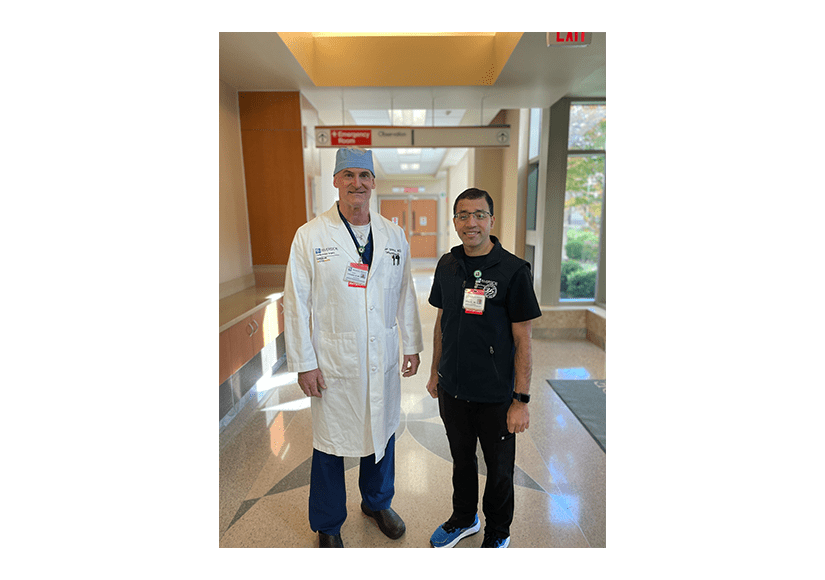
“SABR is a powerful example of how Riverside is transforming lung cancer care through innovation and collaboration,” said Dr. Robert Strange, Cardiothoracic Surgeon with Riverside Cardiothoracic Surgery. “By eliminating multiple procedures and combining them into one day single anesthesia procedure we reduce stress and uncertainty for our patients and offer them the best possible chance at early, curative treatment.”
This approach is especially effective for patients with early-stage non-small cell lung cancer (NSCLC) or suspicious lung nodules discovered during routine or incidental imaging. Nodules are often flagged by Riverside radiologists during low-dose CT (LDCT) screenings, or in imaging studies performed during diagnostic center visits, hospital stays, or emergency care. These cases are promptly referred to the Riverside Lung Nodule Clinic, where patients are typically seen within one week by a pulmonologist team for evaluation and care planning.
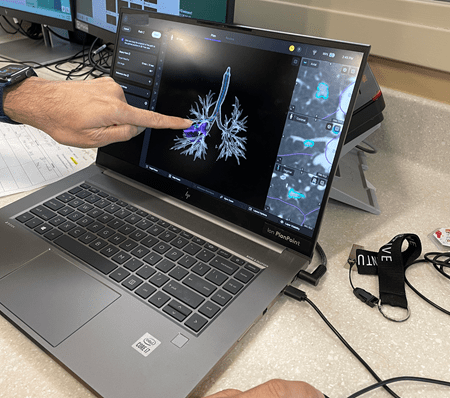
For patients with small or ground glass lung nodules or with a known lung cancer located in the peripheral regions of the lungs, intraoperative identification can be challenging; and in such cases we employ the SABR pathway. For eligible patients undergoing the SABR procedure, the treatment pathway begins with a bronchoscopy. A dye marker is placed closer to the lung nodule to be resected and , the surgical team proceeds immediately with lung resection—most commonly a wedge resection —using minimally invasive techniques such as video-assisted thoracoscopic surgery (VATS) or robotic-assisted surgery. This reduces the overall timeline of care and spares patients the emotional toll of waiting between the two procedures.
“Our patients are waking up with a diagnosis—and their cancer already removed,” said Dr. Som Chalise, Pulmonologist with Riverside Pulmonology Specialists. “That’s a remarkable shift in how we care for our patients facing early-stage lung cancer.
Most patients spend a few days recovering in the hospital after SABR, with support from Riverside’s care teams and, when appropriate, pulmonary rehabilitation to strengthen lung function. With fewer procedures and less time under anesthesia, many patients feel better, faster—and are able to return to their normal activities more quickly.
To learn more about SABR, visit riversideonline.com/lung.