Reducing Risk of Stroke without Blood Thinner Medications
The Left Atrial Appendage closure procedure using the WATCHMAN™ device gives patients living with atrial fibrillation (AFib) an alternative way to reduce the risk of stroke instead of taking blood thinner medications. Riverside’s cardiac electrophysiologists and structural cardiologists place the WATCHMAN™ device inside the heart to seal off the area at highest risk for dangerous blood clots for patients with AFib.
AFib Increases Risk of Stroke
People who have atrial fibrillation (AFib) are 5 times more likely to have a stroke than those without AFib. This 500% increased risk of stroke is because this heart rhythm can cause blood clots to form in an area of the heart known as the Left Atrial Appendage (LAA). Due to the position of this area in the heart, any clot that comes from there can travel directly to the vessels in the brain, potentially blocking the brain’s blood supply and causing a stroke. In fact, 90% of strokes caused by blood clots from the heart are caused by LAA clots.
Most patients with AFib are put on medications, commonly known as blood thinners, to decrease the risk of clots. Historically this medication was warfarin, but there is a new group of anti-coagulation (clot prevention) medications used that include Pradaxa, Xarelto and Eliquis. For patients with AFib, taking blood-thinner medications can reduce the risk of stroke by approximately 50 – 60%. These medications do increase the risk of bleeding as they prevent clots, but some people are not able to tolerate them.
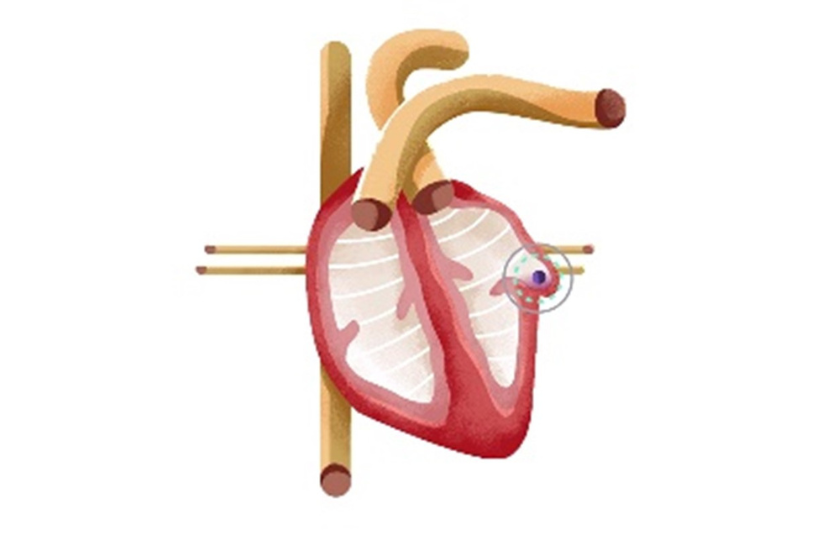
For patients unable to take or tolerate blood thinners, a procedure known as a Left Atrial Appendage Closure (LAA Closure) can be done to reduce the risk of stroke. In this catheter-based procedure the WATCHMAN™ device is placed inside the heart to seal off the LAA from the rest of the heart.
How is the WATCHMAN Procedure Done?
The cardiac electrophysiologist or structural cardiologist uses a catheter device to go through the vein, usually starting near the groin area with the femoral vein, to go up to the left atrial appendage area inside the heart. Utilizing both cardiac ultrasound and x-ray technology, the physician is able to navigate to the precise location for the device to be placed.
The WATCHMAN™ device is approximately the size of a quarter. It is folded compactly so it can travel through the catheter and be implanted into the heart to seal off the left atrial appendage.
The whole procedure takes 1 – 2 hours, and the patient is asleep during that time. The device is permanent and remains in the heart. The patient usually spends one night in the hospital.
What Happens After the Procedure?
After the patient is discharged from the hospital, they continue to take medication to prevent clotting while the heart heals from the procedure. The physician will discuss the exact medication regimen with the patient. During this time, the patient’s heart will naturally grow a tissue barrier across the implant to form the barrier sealing off the left atrial appendage.
Approximately 4 – 6 weeks after the procedure, the physician will get additional images of the heart to confirm the tissue has grown over the device. Once the healing and tissue barrier is confirmed, the physician will start a different medication regimen. Eventually the patients come off the additional medications, but some may remain on aspirin for the rest of their lives.
Who is Eligible for the WATCHMAN™ Device?
Not every patient is eligible for the WATCHMAN™ device. Individuals may be candidates for the procedure if they:
- Have atrial fibrillation not caused by a heart valve problem (known as non-valvular AFib);
- Have elevated stroke risk due to AFib;
- Are on or have been prescribed blood thinning medications; and
- Are unable to take blood thinners long term due to any of the following:
- Problems with or history of bleeding
- High risk of falls
- Have increased risk of kidney (renal) failure
- Have potential drug interactions due to other medical conditions
- Have a job or lifestyle where long-term anti-coagulation medications aren’t ideal
- Inability to adhere to blood thinner treatment
- History of blood disorders or certain cancers
Eligible patients who are considering the procedure then have advanced imaging tests done in order to assure their individual anatomy is compatible with the device.
Individuals are encouraged to speak with their cardiologists to see if this is an appropriate treatment option for their individual situation.
To Refer a Patient or Schedule an Appointment
To refer a patient to Riverside’s Structural Heart Program or to Riverside’s Heart Rhythm Program, please call 757-594-2074 or make the ambulatory referral to structural cardiology or cardiac electrophysiology in iCare.
If you have been referred to Riverside’s Structural Heart Program or to Riverside’s Heart Rhythm Program, please call 757-594-2074 to schedule an appointment. Physician referrals are required.
Locations
Riverside Cardiology Specialists – Newport News
12200 Warwick Blvd., Suite 590B
Newport News, VA 23601
757-594-2074
Riverside Cardiology Specialists – Gloucester
7544 Hospital Drive, Building A, Suite 202
Gloucester, VA 23061
757-594-2074