Chronic pain from osteoarthritis or tendinopathy can wear down even the most resilient people—especially when traditional treatments like NSAIDs or physical therapy haven’t worked. If you’re hoping to avoid surgery, platelet-rich plasma (PRP) injections offer a modern alternative with encouraging outcomes for many patients.
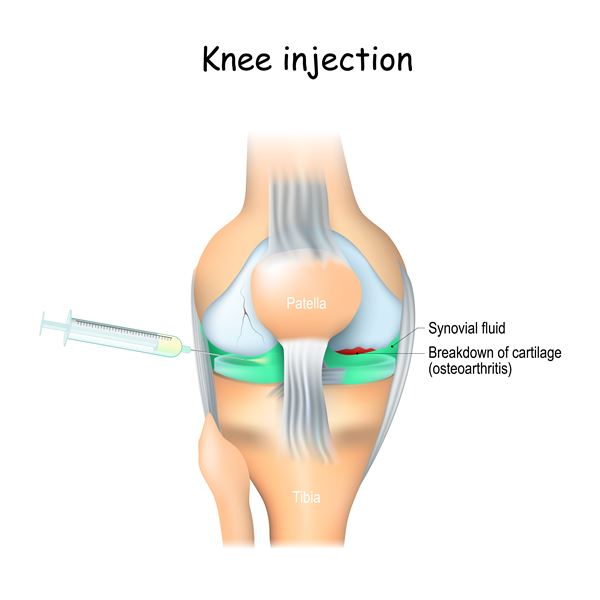
“PRP treatment uses your own blood to help reduce pain, improve joint function and possibly slow, stop or even repair your cartilage damage,” says Orthopedic Surgeon Barbaro J. Perez, M.D., with Riverside Orthopedic and Sports Medicine Specialists in Gloucester. “We separate the platelets and use them to create a solution that includes a variety of healing factors. Then, we inject this blend into the area of your body that is suffering from tendinopathy or osteoarthritis.”
What Are PRP Injections?
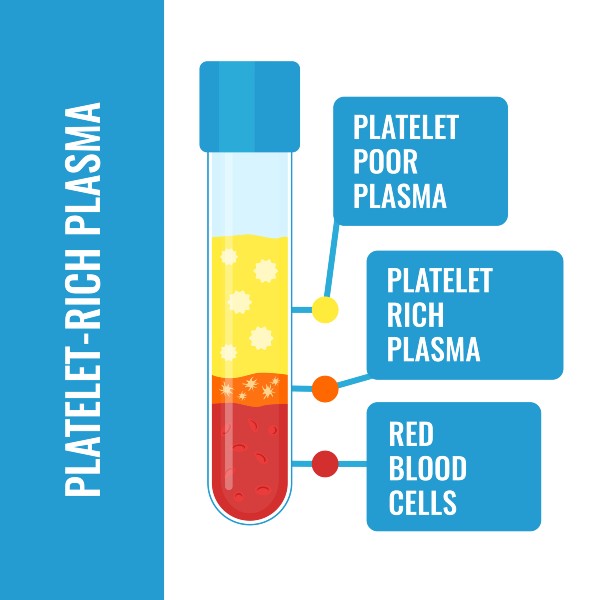
Platelet-rich plasma therapy involves concentrating platelets from a small blood sample and injecting that enriched plasma directly into damaged tissues. Platelets play a central role in healing as they release growth factors and proteins that encourage tissue repair and reduce inflammation.
PRP is considered a regenerative medicine technique and has been widely used in sports medicine, orthopedics and even cosmetic and dental fields. It’s not a cure, but for the right patient, it may help reduce pain and improve mobility.
What Conditions Can PRP Treat?
While research is still ongoing, PRP has shown promise in treating:
- Mild to moderate osteoarthritis, especially of the knee, hip and shoulder
- Chronic tendinopathies, such as tennis elbow, Achilles tendinitis and rotator cuff injuries
- Ligament sprains and muscle strains
- Plantar fasciitis
- Post-surgical healing (in some cases)
It’s important to note that PRP is not typically recommended for complete tendon tears, severe arthritis with advanced joint damage or structural instability that would otherwise require surgical repair.
Who Is a Good Candidate for PRP?
PRP therapy may be right for you if:
- You’ve had persistent joint or tendon pain for at least 3-6 months
- Conservative treatments like NSAIDs or physical therapy haven’t helped
- You’re sensitive to medications like ibuprofen or corticosteroids
- You want to delay or avoid surgery
- You have mild to moderate damage, rather than severe degeneration
“PRP doesn’t work for everyone, and it isn’t a cure, but many Riverside patients have experienced an improvement in their symptoms after PRP injections,” Dr. Perez notes.
Who Should Avoid PRP?
You may not be eligible for PRP if you have:
- A current infection or active cancer
- Low platelet count or a bleeding disorder
- Anemia or significant chronic illnesses
- Are pregnant
- Are on blood thinners and cannot stop them temporarily
- Have a bovine allergy (if using PRP kits that contain animal-derived materials)
How PRP Injections Work: Step-by-Step
While PRP is an outpatient procedure, preparation is key. You’ll need to avoid NSAIDs and certain medications ahead of time. Your orthopedic specialist will provide specific guidance.
Before the Procedure:
- Stop taking NSAIDs at least 7 days prior
- Discontinue corticosteroids 2-3 weeks before
- Avoid blood thinners for 5 days prior, if medically safe
- Hydrate well the day before
The Procedure (45-90 minutes total):
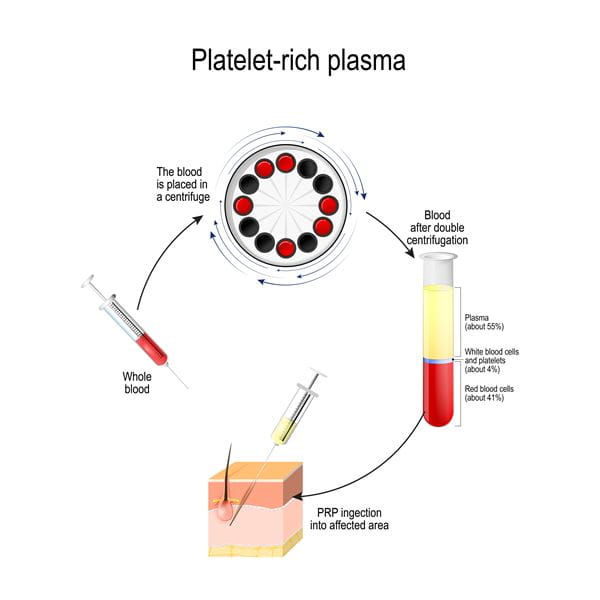
- Blood draw – A small amount of blood is taken from your arm.
- Platelet concentration – The blood is spun in a centrifuge to isolate platelets.
- Injection – The PRP is injected into the targeted joint, tendon or ligament using ultrasound or fluoroscopic guidance if needed.
“If your doctor decides to give you several injections, we will only draw your blood one time. We’ll then freeze the remaining PRP mixture for future injections OR we will draw your blood before each injection to guarantee the PRP mixture is fresh,” explains Dr. Perez.
What to Expect After a PRP Injection
You’ll likely experience soreness or swelling in the injected area for 2-3 days. This is part of your body’s natural healing response. Full healing may take weeks to months depending on the condition and treatment site.
Post-PRP Care:
- Rest the area and avoid heavy activity for a few days
- Apply cold packs for 10–20 minutes several times daily
- Use non-NSAID pain relievers if prescribed
- Resume physical therapy after your provider gives the green light
- You may need temporary support like a brace, sling or crutches
How Effective Is PRP?
Research into PRP is ongoing. The American Academy of Orthopaedic Surgeons (AAOS) and organizations like Johns Hopkins Medicine suggest that while PRP shows potential, it’s not yet a universal solution and not all insurance plans cover it.
Still, many patients report meaningful reductions in pain and stiffness, especially when PRP is used in conjunction with:
- Physical therapy
- Weight management
- Joint stabilization exercises
- Healthy lifestyle changes
Is PRP Right for You?
If you’re seeking a non-surgical option to manage persistent joint or tendon pain, platelet-rich plasma therapy may offer the relief you need. While it’s not for everyone, PRP has helped many Riverside patients reduce their pain, regain mobility and return to the activities they love.
Talk to your orthopedic specialist to find out if PRP injections are appropriate for your condition and health history.
To schedule an appointment to discuss whether platelet-rich plasma injections are right for you, contact Riverside Orthopedic and Sports Medicine Specialists today.